Blanock had come across a live stream of a community meeting to discuss rare cancers that were occurring with alarming frequency in south-western Pennsylvania, where she lives.
Between 2009 and 2019, five other students in Blanock’s school district were also diagnosed with Ewing’s sarcoma. (The region saw about 30 overall cases of the cancer during that time.) In the video, health experts and residents were talking about whether the uptick in illnesses was related to fracking. Blanock was riveted.

 Health Glance
Health Glance



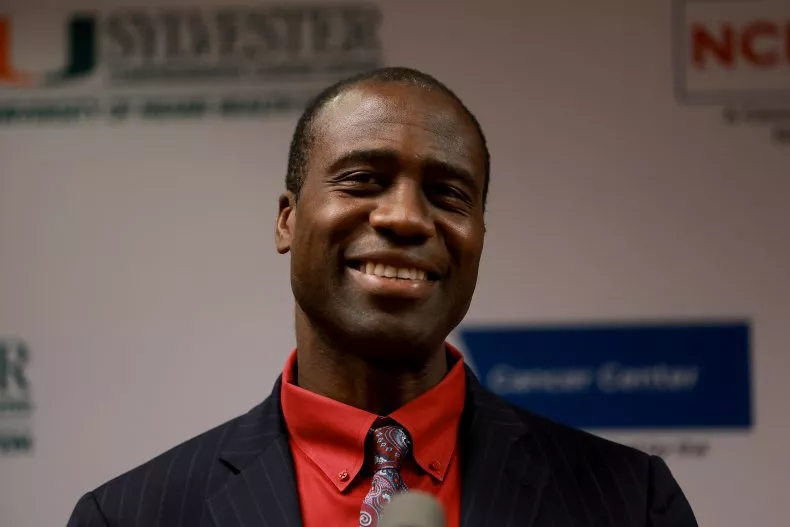 Florida Surgeon General Joseph Ladapo is raising alarms about what he sees as the risk of potential cancer posed by COVID vaccines.
Florida Surgeon General Joseph Ladapo is raising alarms about what he sees as the risk of potential cancer posed by COVID vaccines.
































